Researchers at UTSA are developing a less invasive approach to treating Parkinson’s disease. Using magnetic nanoparticles and alternating magnetic fields, Dr. Gabriela Romero Uribe, a professor of Biomedical and Chemical Engineering, is spearheading research efforts into more targeted and effective treatments.
Current methods for treating Parkinson’s disease involve drug treatments that are restricted by the blood-brain barrier or implants that may damage tissue. Uribe voiced belief that MNP-based treatment can circumvent these obstacles, providing a wireless solution that can be toggled on and off and direct compounds to specific sections of the brain.
“Just [think] about not taking drugs ever to cure any disease because you have this powerful tool,” Uribe said.
MNP-based treatment works by delivering iron-based nanoparticles to the brain via injection or through the nose. These nanoparticles carry compounds altering nerve activity and are coated with a heat-sensitive polymer. When exposed to harmless alternating magnetic fields, the nanoparticles heat up and break down the polymer coating, releasing the compounds.
While Uribe says that MNP-based treatment offers exciting prospects in treating Parkinson’s disease, she acknowledges that more experimenting needs to be done before establishing it in practice. According to her, tests have so far revealed few consequences, yet she anticipates that the brain may reject higher concentrations of iron should more nanoparticles be needed.
“Our brain produces the kind of [iron] particles that we actually are putting in the brain,” Uribe said. “I wouldn’t be surprised, if we need to activate a larger part of the brain and use more material, that the brain [will want] to exclude these foreign particles.”
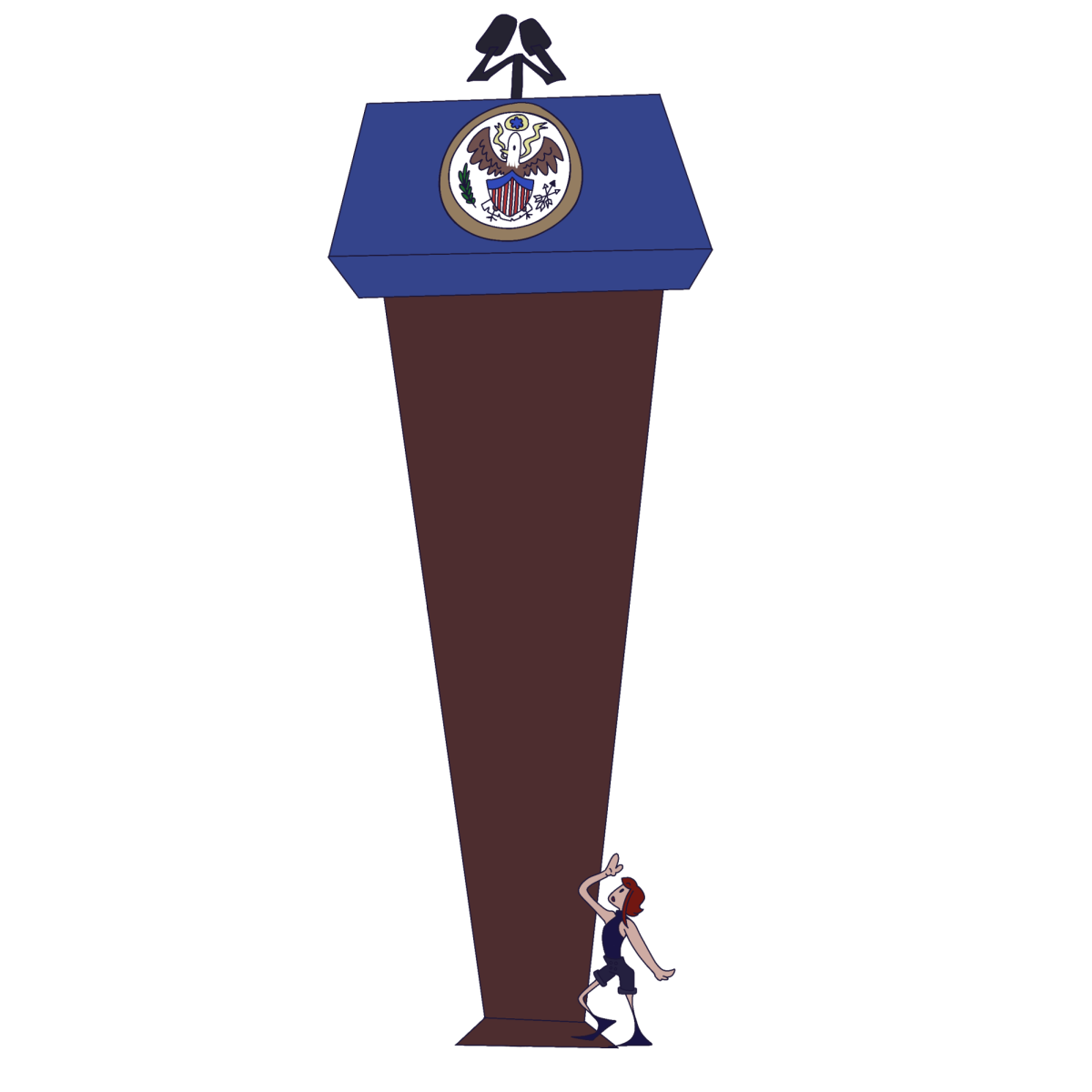
While funding remains “one of the biggest limitations” in fully implementing MNP-based treatment, Uribe anticipates help will come in the form of the UTSA and UT Health San Antonio merger. Input from clinicians, she says, may prove useful in research efforts.
“The merger definitely will open that door even wider to have collaborations with physicians and with clinical researchers,” Uribe said. “Having clinicians’ input when you are developing technology like this is essential. You may think of something and explore it in the lab, but maybe it’s not practical.”
With new technologies and incoming opportunities from the historic merger, Uribe voiced confidence in nanotechnology’s growing role in health care. She urges for more research initiatives on the brain, pointing out that other areas of health have seen developments while neuroscience has lagged behind.
“They should keep exploring this area. We need to speed up the development of medical technologies in the brain,” Uribe said. “It’s particularly important also for other reasons as the cure of cancer and other diseases has evolved.”
Possible useful findings for future research is another factor that drives Uribe’s work.
“All research is successful, even if our research does not produce commercial products,” Uribe said. “At this moment, it is producing new knowledge, and that new knowledge will serve future generations to develop or to innovate technologies.”
Nanotechnology’s applications in health may only be recently emerging, but Uribe and her team will continue contributing to UTSA’s efforts in exploring its uses.